The health effects associated with traumatic brain injury can be cognitive, behavioral, emotional, motor, and somatic. These symptoms vary in persons and are dependent on injury location and severity, as well as prior medical history. Motor, sensory, and somatic symptoms may include headaches, fatigue, sleep disturbance, changes in vision, dizziness, chronic pain, and balance issues.[1]
Mild traumatic brain injury is caused by direct or indirect biomechanical forces to the head that have the potential to cause a spectrum of injury, varying from transient cellular dysfunction to structural damage. This spectrum of mild traumatic injury produces cognitive impairment in the days following injury; however, substantial recovery is generally expected by three months; and group studies usually show no lingering cognitive deficits.[2] Yearly, it is estimated that 3.6 million people in the United States suffer a mild traumatic brain injury, and 400,000 sustain moderate or severe traumatic brain injury.[3] It is understood that traumatic brain injury is a spectrum from mild traumatic brain injury, moderate traumatic brain injury, and severe traumatic brain injury, defined by length of unconsciousness and length of post-traumatic amnesia. These categories have significantly different prognoses as to disability and death.
The definition of mild traumatic brain injury, as defined by the World Health Organization, is the following:
“MTBI is an acute brain injury resulting from mechanical energy to the head from external physical forces. Operational criteria for clinical identification include: (i) 1 or more of the following: confusion or disorientation, loss of consciousness for 30 minutes or less, post-traumatic amnesia for less than 24 hours, and/or other transient neurological abnormalities such as focal signs, seizure, and intracranial lesion not requiring surgery; (ii) Glasgow Coma Scale score of 13–15 after 30 minutes post-injury or later upon presentation for healthcare. These manifestations of MTBI must not be due to drugs, alcohol, medications, caused by other injuries or treatment for other injuries (e.g. systemic injuries, facial injuries or intubation), caused by other problems (e.g. psychological trauma, language barrier or coexisting medical conditions) or caused by penetrating craniocerebral injury.”
The Assistant Secretary of Defense defines mild traumatic brain injury for its providers as a loss of consciousness of 0-30 minutes, post-traumatic amnesia less than 24 hours, and alterations in mental status less than 24 hours beginning immediately and related to trauma of the head. This definition includes symptoms that “would include looking and feeling dazed and uncertain of what is happening, confusion, difficulty thinking clearly or responding appropriately to mental status question, and/or being unable to describe events immediately before or after the trauma event” with no clinically relevant findings on diagnostic imaging that would require further testing. In fact, despite neuroimaging research there is “inadequate evidence to recommend any particular neuroimaging modality or technique for routine clinical use that may aid in the diagnosis and/or direction of care for patients with symptoms attributed to mild traumatic brain injury”.[4] In the absence or transient loss of consciousness, and no clinical evidence of post-traumatic amnesia, is consistent with a mild traumatic brain injury.[5]
The Glasgow Coma Scale (GCS) is a clinical tool used to describe and assess the level of coma, monitor change in the state of coma, and indicate the severity of an illness. It also serves as a triage tool for patients who have sustained head trauma. A GCS score of 13-15 indicates mild head trauma, 9-12 indicates moderate head trauma, and less than or equal to 8 indicates severe head trauma.[6]
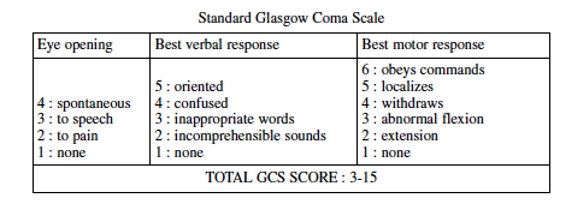
Patients with GCS scores of 13-14 have a significantly higher incidence of initial loss of consciousness, skull fractures, and abnormal findings on CT, and are at higher risk of needing an operation compared with individuals scoring a GCS of 15.[7] Ninety-nine percent of patients with a GCS score of 13-15 have good recovery as described by the Glasgow Outcome Scale.[8]
| CATEGORY | RESPONSE | COMMENTS |
|---|---|---|
| Good recovery | Normal life, minor neurological and psychological deficits. | Family relationships, leisure activities. |
| Moderate disability | Disabled (hemiparesis, ataxia, dysphasia, personality change, memory, and intellectual deficits) but independent. | Able to use public transportation and work in a sheltered environment. |
| Severe disability | Conscious, disabled, and dependent for support for some activities of daily living. | Physical or mental disability or both. |
| Vegetative state | Awake, marked with cycles of sleeping and wakefulness. | Although the cerebral cortex may be intact, there is an absence of function. |
| Dead | Need to differentiate between death due to primary head injury and death due to complications. |
Outcome after mild traumatic brain injury (mTBI) is generally favorable with broad measures of the Glasgow Outcome Scale and is in the ‘Good Recovery’ category. However, it may require additional measures to differentiate among emotional, behavioral, cognitive, and physical domains.[9] Consistent best evidence suggests that there are no cognitive deficits post-injury beyond 1-3 months in the majority of cases.[10] Other measures have been used to differentiate post-concussion symptoms from similar symptoms in the general population, including the Rivermead and Quality of Life studies. These allow for testing subtle changes related to post-concussive syndrome, as there are long-term impacts of post-concussive syndrome in the mild traumatic brain injury group, with 12-15% of those not returning to work.[11]
Patients with mild traumatic brain injury, characterized by loss of consciousness, alterations of consciousness/mental state, post-traumatic amnesia, and Glasgow Coma Scale, may exhibit intracranial findings on a CT scan that are considered clinically relevant. These cases are classified as “complicated mild traumatic brain injury”. Clinically relevant findings on a CT scan of the head or MRI of the brain might “include contusions, subarachnoid hemorrhage, subdural hematomas, intraventricular hemorrhage, petechial hemorrhage, and epidural hematomas”. In most studies, complicated mild traumatic brain injuries are associated with worse outcomes and “different pathological features on head computed tomography carried different implications for mild traumatic brain injury prognosis to 1 year.[12]
The clinical manifestations of mild traumatic brain injury (mTBI), despite normal imaging results from MRIs and CT scans, can involve reversible or irreversible injury to cells sensitive to the forces exerted on the head by trauma. It is not uncommon for patients to experience persistent symptoms 12 months following a mild TBI. This observation is supported by a study involving 1,154 patients with mild TBI and 299 patients with orthopedic trauma as controls. According to this study, 53% of the participants with mild TBI reported impairments 12 months post-injury, compared to 38% of those with orthopedic trauma. Patients with intracranial abnormalities experienced the poorest outcomes; however, even patients without abnormalities reported issues at 12 months.[13] These findings are corroborated by a systematic review and meta-analysis from 2022, which found that one in three adults with mild TBI who presented to a trauma center exhibited at least mild severity in post-concussive syndromes at 3-6 months.[14]
The utility of advanced imaging, such as MRI with DTI, should not supplant the clinical history, early diagnostic imaging, and findings on physical examination, which include the presence of saccades. However, it can be used as confirmatory evidence in patients with complex medical histories, including those with chronic pain and significant psychological distress.[15]
Patients with mild traumatic brain injury often show evidence of cell death within the white matter on advanced imaging, such as MRI with DTI, that may correlate with the anatomical basis for the diagnosis, symptom, or sign following a brain injury, but should not be viewed as pathognomonic of traumatic brain injury as there may be no diagnosis, symptom, or sign with these findings.[16] However, in cases where there is no objective evidence on clinical examination, there may be utility to further diagnostic testing in patients with chronic pain, history of fatigue, and significant psychological distress as anatomic correlation for the symptoms complained of with findings on MRI with DTI, may then support the clinical diagnosis of complicated, mild traumatic brain injury. There is no reliable evidence on my extensive literature review that supports the need for 24-hour attendant care and long-term facility related care in patients with mild traumatic brain injury with no abnormalities on CT scan or MRI of the brain with findings on advance diagnostic testing including MRI with DTI which is consistent with my clinical experience regardless of the mechanism of injury.[17]
The Archives of Physical Medicine and Rehabilitation published a review article in 2014 tiled “Systematic Review of the Prognosis After Mild Traumatic Brain Injury in Adults: Cognitive, Psychiatric, and Mortality Outcomes: Results of the International Collaboration on Mild Traumatic Brain Injury Prognosis”. After select studies of more than 30 patients with mild traumatic brain injury, 101 studies were reviewed following a screen of 77,914 records. Their conclusion was that “most evidence indicates the presence of cognitive deficits in the first two weeks post-mild TBI and some evidence suggests that complete recovery may take 6 months or a year”.[18] The normal course after a mild traumatic brain injury is “a resolution of symptoms within three months, which is the outcome for a majority of patients,” which includes headache, dizziness, fatigue, irritability, poor memory, concentration difficulties, and depression.
My experience is consistent with the literature, indicating that there is a population of patients following a mild traumatic brain injury who continue to suffer from long-term symptoms consistent with post-concussive syndrome, with clinical signs of neurological white matter damage. As a group, they remain functional and live independently, with symptoms of post-concussive syndrome, and there is no literature to suggest that these patients suffer severe disability that would require long-term institutionalization.
As per the VA Clinical Practice Guideline for Management and Rehabilitation of Post-Acute Mild Traumatic Brain Injury, there is currently no evidence that “supports the use of laboratory, imaging, or physiologic testing for diagnosing mTBI or directing the care of patients with symptoms attributed to mild traumatic brain injury”.[19] That recommendation is based on “systematic evidence review of neuroimaging” that there was only “weak associations seen between DTI and outcomes related to symptom severity and return to work” and “no correlation could be made between white matter hyperintensities” on advance diagnostic techniques and “neuropsychological testing or self-reported fatigue”.[20] There is no reliable evidence that complicated mild traumatic brain injuries, when compared to non-complicated mild traumatic brain injury, perform differently on neuropsychological testing and do the same from a cognitive standpoint at 6-8 weeks post injury.[21] A large study from Finland examined diffusion tensor imaging (DTI) and it showed “that those with mild traumatic brain injuries were significantly more likely to have reduced white matter integrity in a greater number of regions of interest on DTI compared to control subjects…however the white matter changes were not associated with functional outcome” and those with complicated mild traumatic brain injuries did not perform more poorly on any neuropsychological test, did not take longer to return to work, and did not report more post-concussion symptoms compared to uncomplicated mild traumatic brain injury.[22]
Between 40-50% of individuals with a history of mild traumatic injury might experience chronic pain, which is more prominent in patients with mild traumatic brain injury when compared with moderate or severe traumatic brain injury. Following traumatic experiences, including mild traumatic brain injury, psychological distress is not uncommon, and symptoms of post-traumatic stress disorder can occur. Soldiers with “both PTSD and mild TBI are at greater risk for various post-concussive symptoms following injury than those with either PTSD or mild TBI alone. Antidepressants for symptoms of PTSD should be used for at least 12 weeks before changing to another therapeutic option. A small study supports the utility of an 8-week residential treatment program for veterans with a history of PTSD and a history of TBI.
[1] CDC. U.S. Department of Health and Human Services. Report to Congress, Traumatic Brain Injury in the United States: Epidemiology and Rehabilitation. https://www.cdc.gov/traumaticbraininjury/ pdf/TBI_Report_to_ Congress_Epi_and_Rehab-a.pdf
[2] Belanger, Vanderploeg. The neuropsychological impact of sports-related concussion: a meta-analysis. J. Int. Neuropsychol. Soc. (2005), 11, 345-357; Belanger, Curtiss, Demery, et al. Factors moderating neuropsychological outcomes following mild traumatic brain injury: a meta-analysis. J. Int. Neuropsychol. Soc. 11, 215-227.
[3] Centers for Disease Control and Prevention. Traumatic brain injury Heads up. 2019: Https://www.cdc.gov/headsup. Accessed 3/19/23.
[4] VA/DoD Clinical Practice Guideline for the Management and Rehabilitation of Post-Acute Mild Traumatic Brain Injury. Version 3.0-June 2021
[5] This definition is per the diagnostic criteria by the WHO Collaborating Center Task Force Mild TBI
[6] Sternback. The Glasgow Coma Scale. J. Emergency Med., 2000, 19: 67-71; Matis, Birbilis. The Glasgow Coma Scale-a brief review Past, present, future. Acta neurol. Belg. 2008, 108, 75-89.
[7] Gomez, Lobato, et al. Mild head injury: differences in prognosis among patients with a Glasgow Coma Scale score of 13-15 and analysis of factors associated with abnormal CT findings. British Journal of Neurosurgery. 10:5, 453-460.
[8] McNett. A Review of the Predictive Ability of Glasgow Coma Scale Scores in Head-Injured Patients. Journal of Neuroscience Nursing. Vol. 39, No.2, April 2007.
[9] Shukla, Devi, et al. Outcome measures for traumatic brain injury. Clinical Neurology and Neurosurgery. Clinical Neurology and Neurosurgery 113 (2011) 435-441.
[10] Carroll, Cassidy, et al. Prognosis for Mild Traumatic Brain Injury: Results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury: J Rehabil Med 2004: Suppl. 43: 84-105.
[11] Petchprapai, Winkelman. Mild Traumatic Brain Injury: Determinanats and Subsequent Quality of Life. A Review of Literature. Journal of Neuroscience Nursing. Vol. 39, No. 5, October 2007.
[12] Yuh, et al. JAMA Neurology-Original Investigation. Pathological Computed Tomography Features Associated with Adverse Outcomes After Mild Traumatic Brain Injury. A TRACK-TBI Study with External Validation in CENTERE-TBI. September 2021. Volume 78, Number 9.
[13] Nelson, et al. Recovery After mild traumatic brain injury in patients presenting to US Level 1 Trauma Centers: A transforming research and clinical knowledge in traumatic brain injury (TRACK-TBI) Study. JAMA Neurol. 2019; 76(9): 1049-1059.
[14] Cancelliere, et al. Post-Concussion Symptoms and Disability in Adults with Mild Traumatic Brain Injury: A Systematic Review and Meta-Analysis. Journal of Neurotrauma. 40:1045-1059 (June 2023).
[15] Tirelli, et al. Saccades and smooth pursuit eye movements in central vertigo. ACTA Otorhinolaryngologica Italica. 2011 Apr; 31(2): 96-102; Tirelli, et al. Saccades and smooth pursuit eye movements in central vertigo; Mani, Asper, Khuu. Deficits in saccades and smooth-pursuit eye movements in adults with traumatic brain injury: a systematic review and meta-analysis. Brain Injury. DOI: 10.1080/02699052.2018.1483030
[16] Panenka, Lange, et al. Neuropsychological Outcome and Diffusion Tensor Imaging in Complicated versus Uncomplicated Mild Traumatic Brain Injury. PLOS ONE. April 27, 2015.
[17] Cooper DB, Vanderploeg RD, Armistead-Jehle P, Lewis JD, Bowles AO. Factors associated with neurocognitive performance in OIF/OEF servicemembers with postconcussive complaints in postdeployment clinical settings. J Rehabil Res Dev. 2014;51(7):1023-34; Mac Donald CL, Johnson AM, Wierzechowski L, Kassner E, Stewart T, Nelson EC, et al. Prospectively assessed clinical outcomes in concussive blast vs nonblast traumatic brain injury among evacuated US military personnel. JAMA Neurol. 2014;71(8):994-1002; Belanger HG, Proctor-Weber Z, Kretzmer T, Kim M, French LM, Vanderploeg RD. Symptom complaints following reports of blast versus non-blast mild TBI: Does mechanism of injury matter? Clin Neuropsychol. 2011;25(5):702-15
[18] Carroll, Cassidy, et al. Review Article: Systematic Review of the Prognosis after Mild Traumatic Brain Injury in Adults: Cognitive, Psychiatric, and Mortality Outcomes: Results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Archives of Physical Medicine and Rehabilitation. 2014; 95(3 Suppl 2): 3152-73)
[19] VA/DoD Clinical Practice Guideline for the Management and Rehabilitation of Post-Acute Mild Traumatic Brain Injury. Version 3.0-June 2021. https://www.healthquality.va.gov/guidelines/Rehab/mtbi/VADoDmTBICPGFinal508. pdf
[20] Ware JB, Biester RC, Whipple E, Robinson KM, Ross RJ, Nucifora PG. Combat-related mild traumatic brain injury: Association between baseline diffusion-tensor imaging findings and long-term outcomes. Radiology. 2016;280(1):212-9; Miller DR, Hayes JP, Lafleche G, Salat DH, Verfaellie M. White matter abnormalities are associated with chronic post-concussion symptoms in blast-related mild traumatic brain injury. Hum Brain Mapp. 2016;37(1):220-9; Veeramuthu V, Narayanan V, Kuo TL, Delano-Wood L, Chinna K, Bondi MW, et al. Diffusion tensor imaging parameters in mild traumatic brain injury and its correlation with early neuropsychological impairment: A longitudinal study. J Neurotrauma. 2015;32(19):1497-509.
[21] Panenka, Lange, et al. Neuropsychological Outcome and Diffusion Tensor Imaging in Complicated versus Uncomplicated Mild Traumatic Brain Injury. PLOS ONE. April 27, 2015.
[22] Waljas, Huhtala, Iverson, Hartikainen. A Prospective Biopsychosocial Study of the Persistent Post-Concussion Symptoms Following Mild Traumatic Brain Injury. Journal of Neurotrauma. Nov. 2014.

Injury Care Solutions Group (ICSG) provides educational expert content that does not constitute medical advice, diagnosis, treatment, or legal advice or solicitation. ICSG is not a law firm or medical provider. Use of this website does not create a doctor–patient or attorney–client relationship. Do not send PHI through this Website. Attorney references (including references to Ben Martin Law Group) are for convenience only, and are not endorsements, guarantees or attorney advertising. Past results do not predict future outcomes. See Full Disclaimer and Privacy Policy. If deemed attorney advertising: Ben C. Martin, 4500 Maple Ave., Suite 400, Dallas, Texas 75219, licensed by the State Bar of Texas and Pennsylvania.