Neonatal encephalopathy is a “Clinical syndrome of disturbed neurologic function in the first week after birth in an infant born at or beyond 35 weeks of gestation, manifest by a subnormal level of consciousness or seizures, often accompanied by difficulty with initiating and maintaining respiration, depression of tone and reflexes… Hypoxic-ischemic encephalopathy is a subgroup of neonatal encephalopathy”. Hypoxic ischemic encephalopathy is graded mild, moderate, and severe and is best described as below:1
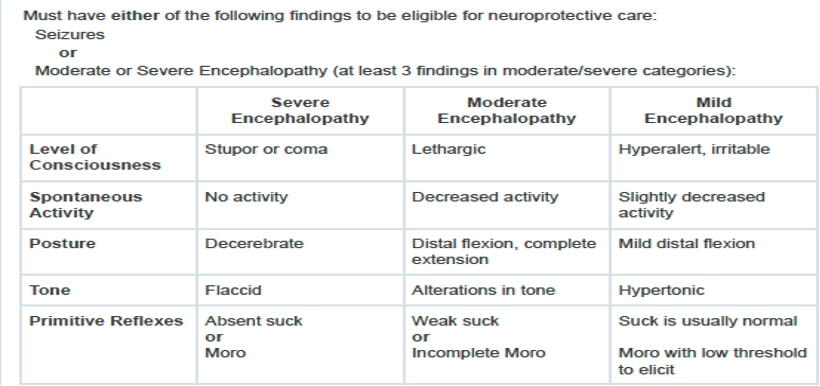
Indications for therapeutic cooling (TH) have been liberalized to include lower grades of HIE as eligible for therapeutic cooling because it represents the only clinically proven neuroprotective intervention that improves outcomes and reduce the risk of cerebral palsy or significant disability in children with either moderate HIE or severe HIE and a recent systemic review revealed that 25% of infants with mild HIT have abnormal outcomes.2
Eligibility for therapeutic cooling includes biochemical criteria and patient characteristics to identify the population at risk for adverse outcomes caused by hypoxia. Biochemical criteria includes two options: 1) Cord blood gas within the first hour of birth which reveals a pH</+ 7 or BE </= -15; 2) Cord blood gas within the first hour of birth which reveals a pH</= 7.15 or BE -10— -14.9 or no blood bas result and Assisted ventilation after birth continued for >/= 10 minutes, or APGAR </=5 and acute perinatal event consistent with complicated delivery including late and/or decelerations, cord prolapse/rupture, uterine rupture, maternal trauma, hemorrhage, cardiorespiratory arrest, shoulder dystocia/nuchal cord, or other event leading to hypoxia. Patient characteristics include >/= 35 0/7 weeks of age and birthweight >1800 grams.
Infants who are <6 hours old and meet the patient characteristics and biochemical criteria AND moderate-severe encephalopathy or seizures qualify.3
Survivors of hypoxic ischemic encephalopathy (HIE) are often left with chronic neurological disability including developmental delay (DD), autism spectrum disorder (ASD), and cerebral palsy (CP). The diagnostic paradigm following complicated deliveries where there was exposure of the newborn to hypoxic condition and then diagnosed with mild, moderate, and severe HIE is changing to early advanced diagnostic imaging of the brain to determine if there are radiologic findings that increased risk for DD, ASD, and CP.
Advance Diagnostic Literature:
[1] Children’s Hospital of Philadelphia Clinical Pathways/Library/Hypoxic-Ischemic Encephalopathy: https://www.chop.edu/clinical-pathway/therapeutic-hypothermia-hypoxic-ischemic-encephalopathy-hie-clinical-pathway
[2] Conway, et al. Mild hypoxic encephalopathy and long term neurodevelopmental outcome- A systematic review. Early Human Development. Early Human Development 120 (2018) 80-87.
[3] Flibotte J, Dysart K, Stoller J, Vossough A, Billinghurst L, Abend N, et al. ICUClinical pathway for therapeutic hypothermia treatment for neonates with hypoxic ischemic encephalopathy (HIE). https://www.chop.edu/clinical-pathway/therapeutic-hypothermia-hypoxic-ischemic-encephalopathy-hie-clinical-pathway. 2021 ; Peebles, et al. Quality Improvement Article: Standardizing neonatal hypoxic ischemic encephalopathy evaluation and documentation practices. Journal of Perinatology. 4 February 2024
[4] Calabrese, MD, Ph.D., et al. Correlating Quantitative MRI-based Apparent Diffusion Coefficient Metrics with 24-month Neurodevelopmental Outcomes in Neonates from the HEAL Trial. Radiology: Vol. 308: Number 3-Sept. 2023.
[5] Im, et al. Volumetric changes in brain MRI of infants with hypoxic-ischemic encephalopathy and abnormal neurodevelopmental who underwent therapeutic hypothermia. Brain Research 1825 (2024) 148703.
[6] Preciado, et al. Prenatal exposure to hypoxic risk conditions in autistic and neurotypical youth: Associated ventricular differences, sleep disturbance, and sensory processing. Autism Research. 2024; 17:2547-2557.
[7] Spencer, et al. Brain volumes and functional outcomes in children without cerebral palsy after therapeutic hypothermia for neonatal hypoxic-ischaemic encephalopathy. Dev Med Child Neurol. 2023; 65:367-375.
[8] Wortinger, et al. Association of Birth Asphyxia with Regional White Matter Abnormalities Among Patients With Schizophrenia and Bipolar Disorders. JAMA Network Open. 2021;4(12): e2139759

Injury Care Solutions Group (ICSG) provides educational expert content that does not constitute medical advice, diagnosis, treatment, or legal advice or solicitation. ICSG is not a law firm or medical provider. Use of this website does not create a doctor–patient or attorney–client relationship. Do not send PHI through this Website. Attorney references (including references to Ben Martin Law Group) are for convenience only, and are not endorsements, guarantees or attorney advertising. Past results do not predict future outcomes. See Full Disclaimer and Privacy Policy. If deemed attorney advertising: Ben C. Martin, 4500 Maple Ave., Suite 400, Dallas, Texas 75219, licensed by the State Bar of Texas and Pennsylvania.