The American Urogynecologic Society and International Urogynecological Association in the 2020 Joint Position Statement on the Management of Mesh-Related Complications for the FPMRS Specialist states:
“Women experiencing mesh complications … should have access to resources and providers who are most able to help. Many women require multiple procedures to address their mesh complications, and for some of these patients, relief is incomplete”
Injury Care Solutions Group has life care planners available who by review of the medical records and by interview with the client will provide future care recommendations based on their skill, knowledge, experience, and training for women who suffer complications including pain, which may include obturator neuralgia, pudendal neuralgia, and pelvic myofascial pain syndrome that are known to be caused by mid-urethral slings that their medical providers have diagnosed.
Stress urinary incontinence affects up to 35% of the US female population, of which approximately 13.5% have had surgical repair over their lifetime . 1 Urethral hypermobility related to decreased urethral support is the most common cause of stress urinary incontinence in women. Stress urinary incontinence is the involuntary loss of urine as a result of a valsalva that may result from a cough or exertion.2 Etiology is most related to soft tissue laxity caused by childbirth. Surgical managements have a common mechanism of action to restore the anatomical support of the bladder neck.
Prior to the widespread use of synthetic slings, the Burch colposuspension procedure was considered the “gold standard” for the treatment of stress urinary incontinence. The Burch elevates the bladder neck and the proximal urethra with non-absorbable sutures lateral to the bladder neck to the Cooper’s ligament (Figure 1). .3 Cochrane review of 55 trials and 5417 women revealed an overall continence rate at one year of 85-90% and 70% at five years. Chronic pain is a rare outcome, with the Burch and long-term overactive bladder symptoms and bladder pain syndrome being less than 1%.4
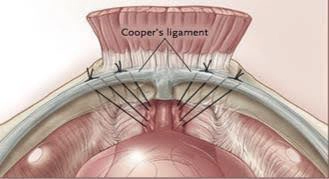
fig-1-Burch Colposuspension
Autologous fascia pubovaginal slings have been a long-standing treatment of stress urinary for over a century with either rectus fascia or fascia lata used to create a hammock to support the bladder neck and urethra (Figure 2).5 Outcomes for stress urinary incontinence with autologous fascia pubovaginal slings have similar success rate between synthetic slings but fell out of favor because it takes 107.6 minutes versus 20.6 minutes for synthetic slings and there is a greater risk of bladder obstruction with autologous slings (8.5% vs. 0.9%) in a study of 436 patients.6 Autologous slings have been seeing a recent resurgence given the low rate of adverse events without the unique complications of synthetic materials that include vaginal erosion and urethral damage. The autologous pubovaginal sling continues to be a valuable surgical option for those with stress urinary incontinence as primary treatment for those who do not want to accept the risks of polypropylene and those who have previously suffered complications caused by synthetic midurethral slings, such as erosions into the urethra and vagina or bladder, or suffered other complications, including urethrovaginal fistulas.7
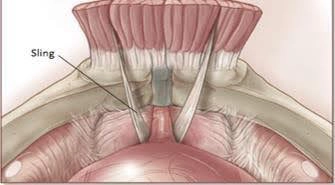
Figure 2. Fascial Sling
There are multi-incision transobturator slings (Figure 3), multi-incision retropubic slings (Figure 4), and single-incision mini-slings. The arms of multi-incision slings pass out of the pelvis while single incision mini-slings have anchors or other tissue fixation designs into the obturator internus muscle to suspend the vaginal component, which acts to support the urethra to prevent incontinence. (The anatomic structures impacted by the polypropylene will be discussed below.)
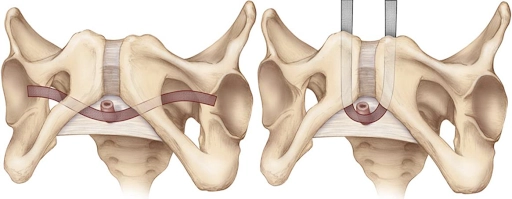
Figure 3: Transobturator Sling Figure 4: Retropubic sling

Figure 5 Single incision mini-sling (Tissue fixation into the obturator internus muscle)
Mid-urethral polypropylene synthetic slings now dominate the surgical management of stress urinary incontinence. The introduction of the retropubic Tension-free Vaginal Tape in 1998 by Ethicon was followed by other designs from multiple manufacturers that include the transobturator slings and mini-slings that led to a “drastic increase” in numbers and rates of sling placements for SUI”.8 Manufacturing companies brought new devices to the market using the FDA 510(k) process of clearance of devices which requires that the new device is substantially equivalent to another legally approved device that is referred to as the predicate.9 The most recent position of the FDA regarding polypropylene mid-urethral slings for the treatment of stress urinary incontinence is that “The safety and effectiveness of multi-incision slings is well-established in clinical trials that followed patients for up to one year” and “The safety and effectiveness of mini-slings for female stress urinary incontinence have not been adequately demonstrated. “.10
In 2017, Rac et al. reported that academic tertiary care centers have decreased their use, and the number of sling revision surgeries for complications from these devices has increased threefold at these centers, while at the same time, the use of autologous slings increased.11 Recent literature from studies designed to mitigate the effect of study subject dropout have found that multi-incision slings and single-incision slings have a 14% incidence of groin pain at three years, and that revision rates are at 7.9% at 17 years and over half of these revision surgeries involve diagnoses that include fistulas and pain.12 Mesh-related complications that occur over time are related to the chronic foreign body reaction.
Polypropylene mid-urethral slings are devices that intend to be permanently implantable devices, and like metal and ceramic implantable devices, will always trigger an acute then a chronic, persistent inflammatory response that varies depending on the material. The acute and chronic
Foreign body reaction is an attempt of the body to isolate the foreign body from the host tissue, similar to the formation of a granuloma. This process is mediated by multinucleated giant cells that depend on the type of biomaterial.13 A strong pro-inflammatory response and pro-fibrotic mechanism of pain has been implicated as causative of complications, and there are immunological markers that include pro-fibrotic cytokines that correlate with fibrosis and correlate with the likelihood of improvement in pain after mesh removal.14 Mesh-related pain has been characterized by a painful band of mesh that is associated with fibrosis and mesh contraction.15 Complex Regional Pain Syndrome has been implicated in the hernia mesh literature, which may be secondary to direct intraoperative nerve injury or nerve injury due to inflammation or from another to be determined mechanism 16
The International Urogynecology Association Research and Development Committee opinion in 2019 key points is the following: 1) “Pain is a common midurethral mesh complication requiring surgical mesh removal”: 2) Groin pain following a TVT (retropubic sling) may be due to damage to the ilioinguinal nerve; 3) “Damage to the obturator nerve is implicated after transobturator slings”; 4) “Groin pain is believed to be related to obturator nerve damage or entrapment neuropathy”; and 5) “Chronic pelvic pain might develop from pelvic floor muscle spasm, pudendal neuralgia and infection”.17
It is imperative that physicians who take care of musculoskeletal conditions are aware of the diagnoses that are related to mid-urethral slings and that these diagnoses may include pain following mid-urethral sling placement, which may occur acutely following implantation and become chronic or may develop symptoms years after implantation.18 Delayed onset pain can be related to mesh contracture/inflammation, mesh exposure and/or erosion, mesh infection, nerve
1 Markland AD, Richter HE, Fwu CW, et al. Prevalence and Trends of Urinary incontinence in adults in the US, 2001 to 2008. J Urol 2011;186(2):589–93. Oliphant SS, Jones KA, Wang L, et al. Trends over time with commonly performed obstetric and gynecologic inpatient procedures. Obstet Gynecol 2010;116(4):926–31; Wu JM, Matthews CA, Conover MM, et al. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol 2014;123(6): 1201–6.
2 Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29:4–20.
3 Veit-Rubin, Dubuisson, Ford, Dubuisson, Mourad, Digesu. Burch colposuspension. Neurourology and Urodynamics. 2019; 38: 553-562.
4 Karmakar, Dwyer, Murray, Schierlitz, Dykes, Zilberlicht. Long-term effectiveness and safety of open Burch colposuspension vs retropubic midurethral sling for stress urinary incontinence-results from a large comparative study. American Journal of Obstetrics & Gynecology. June 2021.
5 Ghoneim, Rizk. Renaissance of the autologous pubovaginal sling. International Urogynecology Journal 29, 177-178 (2018)
6 Natalin, Riccetto, Pedro, Prudente, Navarrete, Palma. Autologous versus synthetic sling procedure: success and bladder outlet rates. Actas Urologicas Espanolas 2009, 33(2): 154-158.
7 Milose, Sharp, He, Stoffel, Clemens, Cameron. Journal of Urology. Vol . 193, Issue 3, March 2015, 916- 920; Lee, Alhalabi, Zimmern. Long-term outcomes of autologous fascia lata sling for stress incontinence secondary to intrinsic sphincter deficiency. Urological Science 29 (2017) 135-138.
8 Funk, Siddiqui, Pate, Amundsen, Wu. Sling Revision/Removal for Mesh Erosion and Urinary Retention: Long-Term Risk and Predictors. Am J Obstet Gynecol. 2013 Jan; 208(1): 73; Rac, Younger, Clemens, Kobashi, Khan, Nitti, Jacobs, Lemack, Brown, Dmochowski, MacLachlan, Mourtzinos, Ginsberg, Koski, Rames, Rovner. Stress Urinary Incontinence Surgery Trends in Academic Female Pelvic Medicine and Reconstructive Surgery Urology Practice in the Setting of the Food and Drug Administration Public Health Notification. Neurourology and Urodynamics 36:1155-1160 (2017).
9 Ostergard. Vaginal mesh grafts and the Food and Drug Administration. International Urogynecology Journal 21, 1181-1183 (2010).
10 https://www.fda.gov/medical-devices/urogynecologic-surgical-mesh-implants/considerations-about- surgical-mesh-sui
11 Rac, Younger, Clemens, Kobashi, Khan, Nitti, Jacobs, Lemack, Brown, Dmochowski, MacLachlan, Mourtzinos, Ginsberg, Koski, Rames, Rovner. Stress Urinary Incontinence Surgery Trends in Academic Female Pelvic Medicine and Reconstructive Surgery Urology Practice in the Setting of the Food and Drug Administration Public Health Notification. Neurourology and Urodynamics 36:1155-1160 (2017).
12 Dejene, Funk, Pate, Wu. Long-Term Outcomes After Midurethral Mesh Sling Surgery for Stress Urinary Incontinence. Female Pelvic Med Reconstr Surg 2022, 28: 188-193; Abdel-Fattah, et al. Single-Incision Mini-Slings for Stress Urinary Incontinence in Women. NEJM 2022; 386: 1230-43.

Injury Care Solutions Group (ICSG) provides educational expert content that does not constitute medical advice, diagnosis, treatment, or legal advice or solicitation. ICSG is not a law firm or medical provider. Use of this website does not create a doctor–patient or attorney–client relationship. Do not send PHI through this Website. Attorney references (including references to Ben Martin Law Group) are for convenience only, and are not endorsements, guarantees or attorney advertising. Past results do not predict future outcomes. See Full Disclaimer and Privacy Policy. If deemed attorney advertising: Ben C. Martin, 4500 Maple Ave., Suite 400, Dallas, Texas 75219, licensed by the State Bar of Texas and Pennsylvania.